addiction and the brain pdf
Category : PDF
Addiction is a chronic brain disease characterized by compulsive substance use, despite negative consequences. Neuroscience reveals that it alters brain structures, affecting judgment, decision-making, and emotional regulation; Brain imaging shows changes in regions like the prefrontal cortex, basal ganglia, and amygdala. These changes disrupt dopamine systems, driving addictive behaviors. Understanding addiction as a brain disease emphasizes the need for comprehensive treatment approaches.
1.1 Understanding Addiction as a Brain Disease
Addiction is a chronic brain disease characterized by compulsive substance use despite negative consequences. Neuroscience shows it alters brain structures, affecting judgment, decision-making, and emotional regulation. Changes in the prefrontal cortex, basal ganglia, and amygdala disrupt dopamine systems, driving addictive behaviors. This biological basis explains the transition from recreational use to compulsive dependence, emphasizing the need for medical intervention.
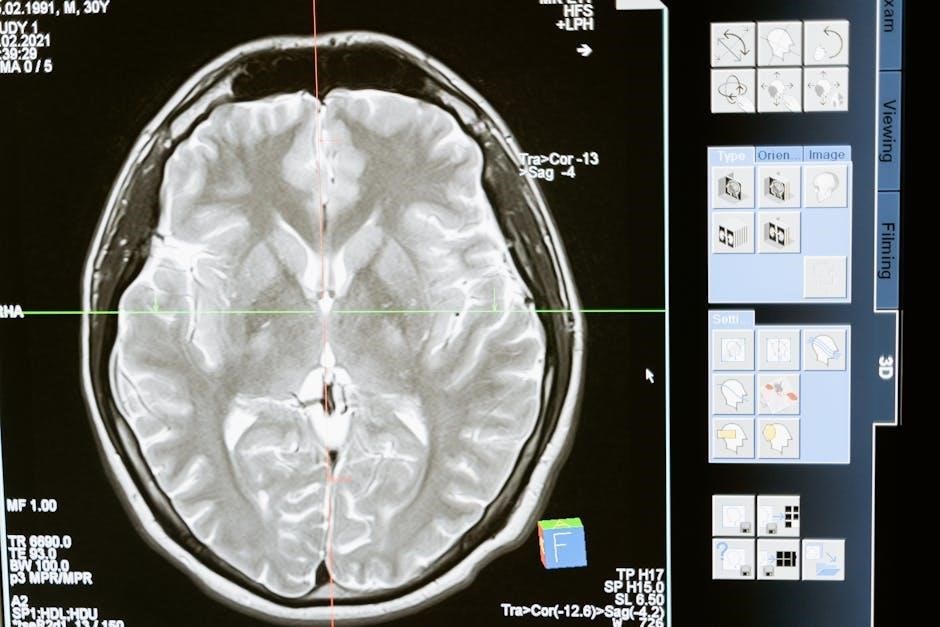
1.2 The Role of Neuroscience in Studying Addiction
Neuroscience has revolutionized the study of addiction by uncovering its biological mechanisms. Advanced neuroimaging techniques like fMRI and MRI reveal how addictive substances alter brain structures, particularly in the prefrontal cortex and basal ganglia. These changes disrupt decision-making, reward processing, and emotional regulation. Neuroscience research informs the development of pharmacological and behavioral treatments, offering hope for combating this chronic brain disease and reducing stigma.
Key Brain Regions Involved in Addiction
Addiction primarily affects the prefrontal cortex, basal ganglia, and amygdala. These regions regulate decision-making, reward processing, and emotional responses. Dysfunctional communication between them drives compulsive behaviors.
2.1 The Prefrontal Cortex and Decision-Making
The prefrontal cortex governs decision-making, impulse control, and rational thinking. Addiction impairs this region, reducing cognitive flexibility and increasing impulsive choices. Chronic substance use damages neural circuits, leading to poor judgment and inability to resist cravings. This dysfunction contributes to the compulsive behavior characteristic of addiction, making recovery challenging without targeted interventions.
2.2 The Basal Ganglia and Reward Processing
The basal ganglia play a crucial role in reward processing, learning, and habit formation. Addictive substances overstimulate this region, releasing excessive dopamine and reinforcing drug-seeking behaviors. Chronic exposure disrupts normal reward pathways, leading to long-term changes in brain circuitry. This hijacking of the brain’s reward system perpetuates addiction, making it difficult to break the cycle without medical intervention.
2.3 The Amygdala and Emotional Regulation
The amygdala, a key structure in emotional regulation, is heavily impacted by addiction. Chronic substance use disrupts its function, leading to heightened stress responses and emotional dysregulation. This imbalance drives the cycle of craving and relapse, as individuals may turn to drugs to cope with overwhelming emotions. Understanding this link is crucial for developing therapies that restore emotional stability and reduce addictive behaviors.

The Neuroscience of Addiction
Addiction fundamentally alters brain chemistry and function, particularly in reward and stress pathways; Neuroscience highlights how substances hijack dopamine systems, leading to long-term changes in brain structure and behavior, perpetuating the cycle of addiction.
3.1 How Addictive Substances Alter Brain Chemistry
Addictive substances trigger excessive dopamine release, altering brain chemistry and reward pathways. Chronic use leads to changes in brain structure and function, particularly in the prefrontal cortex and basal ganglia. This disrupts cognitive and emotional regulation, fostering dependence and compulsive behaviors. Over time, the brain adapts, reducing natural dopamine production and increasing sensitivity to stress.
3.2 The Role of Dopamine in Reward and Addiction
Dopamine is a neurotransmitter central to reward processing and motivation. Addictive substances hijack this system, releasing excessive dopamine and reinforcing pleasurable behaviors. Over time, the brain adapts by reducing dopamine receptors, leading to tolerance and cravings. This imbalance drives the cycle of addiction, as individuals seek more of the substance to achieve the same dopamine high.

The Addiction Cycle
The addiction cycle consists of three stages: preoccupation/anticipation, binge/intoxication, and withdrawal/negative affect. Each stage progressively alters brain chemistry, reinforcing compulsive behavior and dependence.
4.1 Preoccupation and Anticipation (Craving)
Preoccupation and anticipation are the first stages of the addiction cycle, driven by intense cravings. These cravings stem from alterations in brain reward pathways, particularly dopamine systems, which create a compulsive desire to seek substances. This stage is marked by obsessive thoughts and behaviors focused on obtaining the substance, setting the stage for the cycle to continue. Cravings are often triggered by environmental cues or stress, which activate the brain’s reward and stress circuits, making relapse more likely. Understanding these mechanisms is crucial for developing effective interventions to interrupt the cycle early on. Early intervention can prevent the progression to more severe stages of addiction and improve long-term recovery outcomes.
4.2 Binge/Intoxication and Its Effects on the Brain
Binge or intoxication is the second stage of the addiction cycle, characterized by excessive substance consumption. This phase triggers a surge in dopamine release, primarily in the nucleus accumbens, reinforcing the behavior; Repeated episodes lead to brain changes, including tolerance and dependence, as the brain adapts to the substance’s presence, impairing decision-making and memory functions.
4.3 Withdrawal and Negative Affect
Withdrawal occurs when substance use ceases, triggering physical and emotional distress. This phase is marked by negative affect, including anxiety, irritability, and depression. The brain’s stress systems are activated, and dopamine levels drop significantly, intensifying cravings. Chronic withdrawal can impair emotional regulation and cognitive function, making relapse more likely and perpetuating the addiction cycle.
Neuroplasticity and Brain Changes in Addiction
Addiction induces neuroplasticity, altering brain structure and function through chronic drug use, leading to long-term changes that affect behavior and cognition, with potential for recovery.
5.1 Synaptic Plasticity and Long-Term Adaptations
Synaptic plasticity in addiction involves long-term adaptations where repeated drug exposure strengthens pathways linked to reward and craving, weakening those associated with self-control. This reshaping of neural circuits perpetuates compulsive behaviors, as the brain’s reward system becomes dominated by drug-seeking habits, leading to enduring changes in behavior and cognition that are challenging to reverse.
5.2 The Impact of Chronic Drug Use on Brain Structure
Chronic drug use causes significant changes in brain structure, particularly in regions like the prefrontal cortex, basal ganglia, and amygdala. These alterations impair decision-making, emotional regulation, and reward processing. Long-term drug exposure reduces gray matter volume and disrupts neural connectivity, leading to cognitive deficits and heightened vulnerability to relapse. Such structural changes underscore the profound impact of addiction on brain health and function.
Treating Addiction as a Brain Disease
Treating addiction involves rehabilitation strategies, medications, and cognitive therapies to restore brain function. A comprehensive approach addresses dopamine imbalances and promotes long-term recovery.
6.1 Rehabilitation Strategies and Brain Recovery
Rehabilitation strategies focus on restoring brain function through cognitive-behavioral therapy, medication, and support systems. These approaches target dopamine imbalances and promote neural rewiring. Long-term sobriety, often requiring 4-12 months, allows the brain to heal and recover from addiction-related damage. A comprehensive treatment plan is essential for lasting recovery and improved mental health.
6.2 Pharmacological Interventions for Addiction
Pharmacological treatments, such as methadone and buprenorphine, manage withdrawal and cravings by stabilizing brain chemistry. Medications like naltrexone block dopamine receptors, reducing relapse risk. These interventions help restore normal brain function and support recovery by targeting neurotransmitter imbalances caused by chronic substance use.
6.3 Cognitive-Behavioral Therapies and Neural Rewiring
Cognitive-behavioral therapies (CBT) help individuals recognize and change harmful thought patterns linked to addiction. By addressing triggers and coping mechanisms, CBT promotes neural rewiring, strengthening circuits for self-control and reducing reliance on substances. This approach complements pharmacological treatments, fostering long-term brain recovery and reducing relapse rates by enhancing the brain’s ability to manage stress and emotions without drugs.

The Role of Dopamine in Addiction
Dopamine, a neurotransmitter linked to reward and pleasure, plays a central role in addiction. Addictive substances trigger excessive dopamine release, altering brain reward pathways and driving compulsive drug-seeking behavior.
7.1 The Dopamine System and Reward Pathways
The dopamine system is central to reward processing, motivating behaviors essential for survival. In addiction, drugs hijack this system, releasing excessive dopamine in the nucleus accumbens, reinforcing drug use. Over time, this disrupts natural reward pathways, leading to dependence and compulsive drug-seeking behaviors despite negative consequences. This neurochemical adaptation drives the cycle of addiction.
7.2 Hijacking the Dopamine System: Mechanisms of Addiction
Addictive substances trigger excessive dopamine release, reinforcing drug use. Over time, this disrupts the brain’s reward system, leading to long-term adaptations. The dopamine system is hijacked, creating dependence. Drugs interfere with natural reward processing, causing compulsive drug-seeking behaviors. This neurochemical hijacking underpins the transition from recreational use to addiction, driven by altered dopamine signaling pathways.
7.3 Dopamine Imbalance and Recovery
Chronic drug use disrupts dopamine balance, impairing reward processing and motivation. Recovery involves restoring dopamine system function through neuroplasticity. Cognitive-behavioral therapies and pharmacological interventions aid in rebalancing dopamine levels. Over time, the brain can recover, but full healing requires prolonged sobriety, often 12-18 months, to rebuild neural pathways and normalize dopamine signaling.

Implications for Policy and Public Health
Understanding addiction as a brain disease reduces stigma, enabling effective prevention strategies and policies. Public health initiatives address root causes, improving treatment accessibility and societal outcomes.
8.1 Reducing Stigma Through Education
Education is key to reducing stigma by reframing addiction as a brain disease rather than a moral failing. Neuroscience and neuroimaging reveal brain changes, helping the public understand addiction’s biological basis; This shift in perception encourages compassion, promotes seeking treatment, and supports recovery efforts, fostering a more inclusive and supportive society for those affected.
8.2 Developing Effective Prevention and Treatment Programs
Effective prevention and treatment programs leverage neuroscience insights to address addiction’s root causes. By targeting brain regions involved in reward and decision-making, interventions can reduce risk factors and improve recovery outcomes. Personalized approaches, combining pharmacological and behavioral therapies, enhance long-term success, ultimately reducing the societal burden of addiction and improving public health.

Emerging Research and Future Directions
Emerging research explores neuroimaging advancements and novel therapeutic targets, offering insights into addiction’s neural mechanisms. Future directions include personalized treatments and innovative therapies to combat addiction effectively.
9.1 Advances in Neuroimaging and Brain Mapping
Neuroimaging techniques like functional MRI and PET scans have revolutionized the study of addiction, revealing detailed brain changes; These tools identify altered reward pathways, dopamine imbalances, and structural modifications. Mapping brain activity helps pinpoint biomarkers for addiction, enabling early intervention and personalized treatment strategies. Such advancements are crucial for understanding addiction’s neurobiological basis and improving therapeutic outcomes.
9.2 Potential New Targets for Addiction Treatment
Neuroscience research has identified promising targets for addiction treatment, including dopamine pathway modulation and neuroplasticity enhancement. Emerging therapies aim to repair damaged brain circuits and restore balance to reward systems. Advances in optogenetics and pharmacogenetics offer tailored approaches, targeting specific neural mechanisms. These innovations hold the potential to revolutionize addiction treatment, improving recovery rates and reducing relapse.

The Importance of Understanding Brain Mechanisms
Understanding brain mechanisms in addiction is crucial for developing effective treatments and raising public awareness. Education bridges the gap between neuroscience and societal understanding, empowering individuals to combat addiction more effectively.
10.1 Bridging the Gap Between Neuroscience and Public Awareness
Education is key to translating neuroscience into public understanding, reducing stigma and fostering empathy. By explaining how addiction alters brain function, initiatives like community programs and school curriculums can demystify the disease. Sharing personal stories and scientific insights helps the public grasp the biological basis of addiction, promoting compassion and support for those affected.
10.2 The Role of Education in Combating Addiction
Education is a powerful tool in combating addiction by equipping individuals with knowledge about its brain mechanisms. Schools and communities can implement programs that teach how substances alter brain chemistry, emphasizing long-term consequences. This awareness empowers people to make informed decisions, reducing vulnerability and promoting healthier choices, ultimately aiding in prevention and recovery efforts.
Addiction is a brain disease affecting judgment, decision-making, and emotional regulation. Understanding its impact on brain chemistry, particularly dopamine, is crucial for developing effective treatments and prevention strategies.
11.1 Recap of Key Findings
Addiction is a brain disease altering key regions like the prefrontal cortex, basal ganglia, and amygdala. It disrupts dopamine systems, driving compulsive behaviors. Chronic use causes structural and functional brain changes, impairing judgment and emotional regulation. Neuroscience advances reveal addiction’s neurobiological mechanisms, emphasizing the transition from recreational use to dependence. Understanding these changes is vital for developing effective treatments and prevention strategies.
11.2 The Need for a Comprehensive Approach to Addiction
A comprehensive approach to addiction is essential, integrating medical, psychological, and social interventions. This includes pharmacological treatments, cognitive-behavioral therapies, and education to address both biological and environmental factors. By bridging neuroscience with public awareness, we can reduce stigma and improve outcomes, ensuring a holistic strategy to combat this complex brain disease effectively.